Gum disease and Heart disease
Can your bleeding gums lead to heart disease?
Written by
Deborah Freudenmann BHSc
Gingivitis is the most common and mild oral-dental disease. Gingivitis is characterised by inflammation and bleeding of the gums. This condition usually isn’t painful in its early stages and therefore often goes unnoticed until severe irritation or receding gums occur.
The oral cavity is an open ecosystem, with dynamic balance between the entrances of microorganisms, colonization and the host defenses aimed for their removal. The main cause of gingivitis is biofilm or as the more commonly referred to plaque, a soft, sticky film that forms on the teeth when starches and sugars react with bacteria which are naturally found in the mouth.
Plaque buildup occurs between the teeth and gums, in faulty fillings, poorly cleaned dentures, braces and so forth. If the plaque is not removed within a certain time frame it hardens into tartar, which cannot be removed by brushing or flossing the teeth.
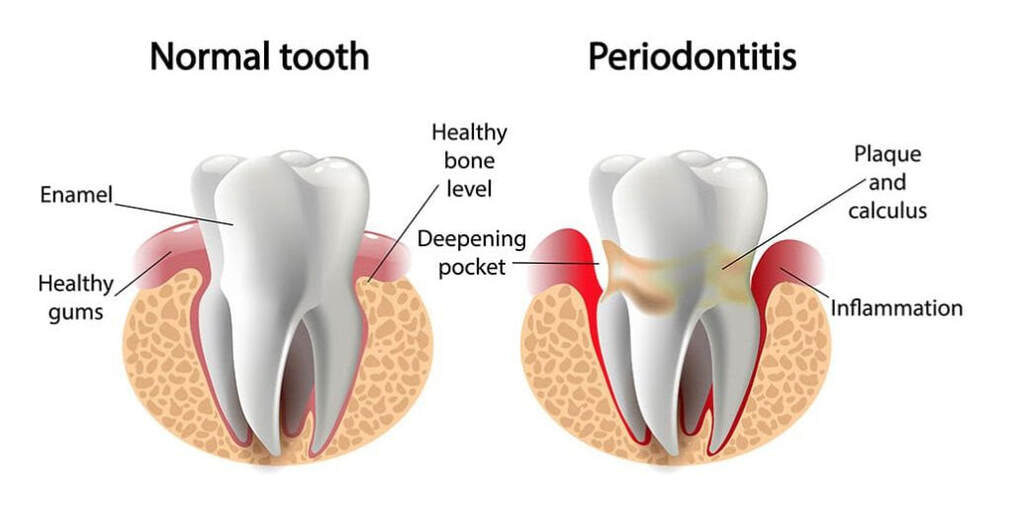
If gingivitis is left untreated, which is often the case due to it going unnoticed it could lead to a more serious condition called periodontitis.
Periodontitis is when the inner gum and bone pull away from the teeth and form pockets. These pockets easily collect bacteria and debris and become infected or abscessed. Bacterial toxins eventually break down the underlying bone and the connective tissue, which holds the teeth in their positions – this results in teeth falling out.
A study "Prevalence of Periodontitis in Adults in the United States: 2009 and 2010" estimates that 47.2 percent, or 64.7 million American adults, have mild, moderate or even severe periodontitis.
Written by
Deborah Freudenmann BHSc
Gingivitis is the most common and mild oral-dental disease. Gingivitis is characterised by inflammation and bleeding of the gums. This condition usually isn’t painful in its early stages and therefore often goes unnoticed until severe irritation or receding gums occur.
The oral cavity is an open ecosystem, with dynamic balance between the entrances of microorganisms, colonization and the host defenses aimed for their removal. The main cause of gingivitis is biofilm or as the more commonly referred to plaque, a soft, sticky film that forms on the teeth when starches and sugars react with bacteria which are naturally found in the mouth.
Plaque buildup occurs between the teeth and gums, in faulty fillings, poorly cleaned dentures, braces and so forth. If the plaque is not removed within a certain time frame it hardens into tartar, which cannot be removed by brushing or flossing the teeth.
If gingivitis is left untreated, which is often the case due to it going unnoticed it could lead to a more serious condition called periodontitis.
Periodontitis is when the inner gum and bone pull away from the teeth and form pockets. These pockets easily collect bacteria and debris and become infected or abscessed. Bacterial toxins eventually break down the underlying bone and the connective tissue, which holds the teeth in their positions – this results in teeth falling out.
A study "Prevalence of Periodontitis in Adults in the United States: 2009 and 2010" estimates that 47.2 percent, or 64.7 million American adults, have mild, moderate or even severe periodontitis.
Some common signs and symptoms of gingivitis include:
What are some of the risk factors for gingivitis?
Medications – certain prescription and over the counter pharmaceutical drugs can create a favorable environment for plaque buildup.
Infections – viral and fungal infections can also adversely affect gum health, infections such as herpes virus, or candida albicans overgrowth.
Disease – These might not be directly associated with the mouth but can adversely affect gum health such as leukemia.
Hormonal changes – Hormonal fluctuations such as pregnancy or menopause can make women more susceptible to gingivitis due to the increased blood supply as well as salivation.
Poor nutrition – A highly inflammatory diet, high sugar intake, processed foods and lacking adequate nutrients such as calcium, vitamin C and B vitamins can increase the risk of developing periodontal disease.
Smoking – smoking diminishes oxygen and nutrient delivery to gum tissue and infers with the regulation of the immune system and inflammation.
Stress – Stress has been linked as a possible cause of gingivitis due to triggering an increase in behaviors including but not limited too smoking, poor oral hygiene, poor diet and so forth.
- Swollen, red or puffy gums
- Pain in the mouth
- Gums that bleed easily when your brush or floss
- Inflamed gums
- Bad breath
- Receding gums
- Tender gums
- Loose tooth or teeth
- Sores in the mouth
- Pus between teeth and gums
What are some of the risk factors for gingivitis?
Medications – certain prescription and over the counter pharmaceutical drugs can create a favorable environment for plaque buildup.
Infections – viral and fungal infections can also adversely affect gum health, infections such as herpes virus, or candida albicans overgrowth.
Disease – These might not be directly associated with the mouth but can adversely affect gum health such as leukemia.
Hormonal changes – Hormonal fluctuations such as pregnancy or menopause can make women more susceptible to gingivitis due to the increased blood supply as well as salivation.
Poor nutrition – A highly inflammatory diet, high sugar intake, processed foods and lacking adequate nutrients such as calcium, vitamin C and B vitamins can increase the risk of developing periodontal disease.
Smoking – smoking diminishes oxygen and nutrient delivery to gum tissue and infers with the regulation of the immune system and inflammation.
Stress – Stress has been linked as a possible cause of gingivitis due to triggering an increase in behaviors including but not limited too smoking, poor oral hygiene, poor diet and so forth.
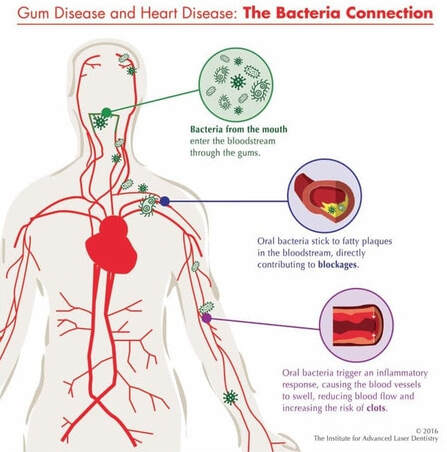 Image from The Institute for Advanced Laser Dentistry, 2016
Image from The Institute for Advanced Laser Dentistry, 2016
Gingivitis and Heart Disease
There is a clear association between gum disease and heart disease. Researchers have established that individuals with periodontal disease are double as likely to have or develop heart disease. Additionally, individuals with high cholesterol and periodontal disease have an even greater risk of developing heart disease. This impacts a lot of people considering just how many people worldwide suffer from cardiovascular conditions as well as periodontal disease.
The link between the two is the role of bacteria from the gums, which has a cascade of inflammatory reactions. The bacteria found in infected gum tissue around the teeth are able to enter the blood stream during normal situations such as chewing or tooth brushing.
The bacteria travel in the blood stream and enter the circulatory system contributing to the formation of cardiovascular diseases. When our bodies have an infection we react with inflammation, swelling or a heat (fever). As oral bacteria travel through the body they trigger a somewhat similar response. Causing the formation of arterial plaque. Oral bacteria’s have been found in patients with atherosclerosis. These deposits can narrow arteries or break off and thus cause complete or partial blockages, ultimately leading to heart attack or stroke.
There is a clear association between gum disease and heart disease. Researchers have established that individuals with periodontal disease are double as likely to have or develop heart disease. Additionally, individuals with high cholesterol and periodontal disease have an even greater risk of developing heart disease. This impacts a lot of people considering just how many people worldwide suffer from cardiovascular conditions as well as periodontal disease.
The link between the two is the role of bacteria from the gums, which has a cascade of inflammatory reactions. The bacteria found in infected gum tissue around the teeth are able to enter the blood stream during normal situations such as chewing or tooth brushing.
The bacteria travel in the blood stream and enter the circulatory system contributing to the formation of cardiovascular diseases. When our bodies have an infection we react with inflammation, swelling or a heat (fever). As oral bacteria travel through the body they trigger a somewhat similar response. Causing the formation of arterial plaque. Oral bacteria’s have been found in patients with atherosclerosis. These deposits can narrow arteries or break off and thus cause complete or partial blockages, ultimately leading to heart attack or stroke.
Conventional Treatment Options
Treatment of gum disease begins with regular brushing and flossing of the teeth. However it is also important to regularly visit a dental hygienist for deep cleaning and monitoring.
There are many other different conventional treatments including mouth rinses, prescription oral rinses, specific toothpastes, antibiotic therapy, surgery and soft tissue grafts.
A 2017 research study was conducted on the efficacy of ozonated water and chlorhexidine mouth rinse against plaque and gingivitis. The study concluded that ozonated water was actually more effective in reducing gingivitis. Furthermore, ozone did not have any side effects contrary to chlorhexidine, which has some side effects.
Treatment of gum disease begins with regular brushing and flossing of the teeth. However it is also important to regularly visit a dental hygienist for deep cleaning and monitoring.
There are many other different conventional treatments including mouth rinses, prescription oral rinses, specific toothpastes, antibiotic therapy, surgery and soft tissue grafts.
A 2017 research study was conducted on the efficacy of ozonated water and chlorhexidine mouth rinse against plaque and gingivitis. The study concluded that ozonated water was actually more effective in reducing gingivitis. Furthermore, ozone did not have any side effects contrary to chlorhexidine, which has some side effects.

Ozone a powerful dental application
Ozone has been used proactively used and researched for dentistry for multiple reasons.
Dental treatment modalities of ozone therapy
(Pattanaik et al., 2011)
Ozone has been used proactively used and researched for dentistry for multiple reasons.
Dental treatment modalities of ozone therapy
(Pattanaik et al., 2011)
- Biofilm purging (Elimination of bacterial pathogens)
- Periodontal pocket disinfection and osseous disinfection
- Prevention of dental caries
Endodontic treatment - Tooth extraction
- Tooth sensitivity
- Tempromandibular joint treatment
- Gum recession (exposed root surfaces)
- Pain control Infection control
- Accelerated healing
- Tissue regeneration
- Controlling halitosis (Bad breath)
- Remineralization of tooth surface
- Teeth whitening (Bleaching)
Ozone treatment has been studied for the removal of oral pathogens. It has been demonstrated that ozone water effectively removes bacteria found on teeth such as Actinomyces naeslundii, Streptococcus mutans and Lactobacillus casei. Additionally ozone water reduces a vast variety of other bacteria and fungi’s present in the mouth.
Ozone water application has various beneficial effects on the oral tissues including remission of various mucosal alterations.
Ozone enhances wound healing and increases the turnover rate of oral cells. It was found that ozonated water applied daily accelerates the healing rate of oral mucosa.
Again the effectiveness of ozone has been proved for the elimination of carious lesions. Deep pockets and fissures in the gums are hard to get too let alone clean properly and hence are highly likely to trap food resulting in bacterial growth. Ozone application in such cases has been found to be highly effective.
Another benefit of ozone is reducing the sensitivity of hypersensitive teeth. Tooth structure loss occurring due to multiple factors such as abrasion, erosion and so forth can cause loss of enamel and dentin thereby causing hypersensitivity. Ozone water and ozone oil application has been found to effectively reduce sensitivity of not only exposed enamel and dentin but also in cases of root sensitivities.
Thus ozone water and ozone oil is highly effective in inhibiting growth in biofilms. Ozone therapy is easy, cost effective, minimally invasive application to dental treatment that truly works.
References
Srikanth, A., Sathish, M., & Sri Harsha, A. (2013). Application of ozone in the treatment of periodontal disease. Journal of Pharmacy and Bioallied Sciences, 5(5), 89. https://doi.org/10.4103/0975-7406.113304
Pattanaik, B., Pattanaik, S., Naitam, D., Jetwa, D., Manglekar, S., & Dani, A. (2011). Ozone therapy in dentistry: A literature review. Journal of Interdisciplinary Dentistry, 1(2), 87. https://doi.org/10.4103/2229-5194.85024
Shoukheba, M. Y. M., & Ali, S. A. (2014). The effects of subgingival application of ozonated olive oil gel in patient with localized aggressive periodontitis. A clinical and bacteriological study. Tanta Dental Journal, 11(1), 63–73. https://doi.org/10.1016/j.tdj.2014.04.001
Tiwari, S., Avinash, A., Katiyar, S., Aarthi Iyer, A., & Jain, S. (2017). Dental applications of ozone therapy: A review of literature. Saudi Journal for Dental Research, 8(1–2), 105–111. https://doi.org/10.1016/j.sjdr.2016.06.005
Jerome Sarris, J. W. (2014). Clinical Naturopathy (2 edition).
Eke, P. I., Dye, B. A., Wei, L., Thornton-Evans, G. O., & Genco, R. J. (2012). Prevalence of periodontitis in adults in the united states: 2009 and 2010. Journal of Dental Research, 91(10), 914–920. https://doi.org/10.1177/0022034512457373
Parkar, S. M., Shah, K., Darjee, N., & Sharma, A. (2017). Efficacy of ozonated water and chlorhexidine mouth rinse against plaque and gingivitis : A randomized clinical trial, 81–85. https://doi.org/10.4103/2468-6859.204702
Sadatullah, S. (2012). Ozonated water an adjunct to tooth brushing and flossing. Myth or reality?, 1847–1852.
Herring, M. F. S. (2016). Illustrated Anatomy of the Head and Neck 5th Edition.
Life Extension. (2013). Disease Prevention and Treatment.
Mathews, M. J., Mathews, E. H., & Mathews, G. E. (2016). Oral health and coronary heart disease. BMC Oral Health, 16(1), 1–10. https://doi.org/10.1186/s12903-016-0316-7
Mozaffarian, D., Benjamin, E. J., Go, A. S., Arnett, D. K., Blaha, M. J., Cushman, M., … Turner, M. B. (2016). Heart disease and stroke statistics-2016 update a report from the American Heart Association. Circulation (Vol. 133). https://doi.org/10.1161/CIR.0000000000000350
Nogales, C. G., Ferrari, P. H., Kantorovich, E. O., & Lage-Marques, J. (2008). Ozone therapy in medicine and dentistry. Journal of Contemporary Dental Practice, 9(4), 1–9.
Grossman, S. C. (2013). Porth’s Pathophysiology: Concepts of Altered Health States.
Huth, K. C., Quirling, M., Lenzke, S., Paschos, E., Kamereck, K., Brand, K., … Ilie, N. (2011). Effectiveness of ozone against periodontal pathogenic microorganisms. European Journal of Oral Sciences, 119(3), 204–210. https://doi.org/10.1111/j.1600-0722.2011.00825.x
Gupta, G., & Mansi, B. (2012). Ozone therapy in periodontics. Journal of Medicine and Life, 5(1), 59–67. Retrieved from http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3307081&tool=pmcentrez&rendertype=abstract
Seidler, V., Linetskiy, I., Hubálková, H., Stanková, H., Smucler, R., & Mazánek, J. (2008). Ozone and its usage in general medicine and dentistry. A review article. Prague Medical Report, 109(1), 5–13.
Bocci, V. V. (1999). Biological and clinical effects of ozone. Has ozone therapy a future in medicine? British Journal of Biomedical Science, 56(4), 270–279. Retrieved from http://mosao2.org/Article – Bocchi
Deborah Freudenmann has a Bachelor of Health Sciences in Naturopathy and is a co-author and teacher of the Functional Medicine Health Coaching program. She has previously completed a Cert. IV in Food Coaching, Diploma in Holistic Massage Therapy and a Diploma in Anatomy and Physiology. Deborah continues to research, write and educate. With a passion for education Deborah has found her interest discovering and assimilating the newest research and finding ways to apply this research. In doing so Deborah continues to investigate and educate people on understanding, finding and resolving the underlying causation of chronic diseases.
(Taken from https://www.trulyheal.com/can-your-bleeding-gums-lead-to-heart-disease/)
Ozone water application has various beneficial effects on the oral tissues including remission of various mucosal alterations.
Ozone enhances wound healing and increases the turnover rate of oral cells. It was found that ozonated water applied daily accelerates the healing rate of oral mucosa.
Again the effectiveness of ozone has been proved for the elimination of carious lesions. Deep pockets and fissures in the gums are hard to get too let alone clean properly and hence are highly likely to trap food resulting in bacterial growth. Ozone application in such cases has been found to be highly effective.
Another benefit of ozone is reducing the sensitivity of hypersensitive teeth. Tooth structure loss occurring due to multiple factors such as abrasion, erosion and so forth can cause loss of enamel and dentin thereby causing hypersensitivity. Ozone water and ozone oil application has been found to effectively reduce sensitivity of not only exposed enamel and dentin but also in cases of root sensitivities.
Thus ozone water and ozone oil is highly effective in inhibiting growth in biofilms. Ozone therapy is easy, cost effective, minimally invasive application to dental treatment that truly works.
References
Srikanth, A., Sathish, M., & Sri Harsha, A. (2013). Application of ozone in the treatment of periodontal disease. Journal of Pharmacy and Bioallied Sciences, 5(5), 89. https://doi.org/10.4103/0975-7406.113304
Pattanaik, B., Pattanaik, S., Naitam, D., Jetwa, D., Manglekar, S., & Dani, A. (2011). Ozone therapy in dentistry: A literature review. Journal of Interdisciplinary Dentistry, 1(2), 87. https://doi.org/10.4103/2229-5194.85024
Shoukheba, M. Y. M., & Ali, S. A. (2014). The effects of subgingival application of ozonated olive oil gel in patient with localized aggressive periodontitis. A clinical and bacteriological study. Tanta Dental Journal, 11(1), 63–73. https://doi.org/10.1016/j.tdj.2014.04.001
Tiwari, S., Avinash, A., Katiyar, S., Aarthi Iyer, A., & Jain, S. (2017). Dental applications of ozone therapy: A review of literature. Saudi Journal for Dental Research, 8(1–2), 105–111. https://doi.org/10.1016/j.sjdr.2016.06.005
Jerome Sarris, J. W. (2014). Clinical Naturopathy (2 edition).
Eke, P. I., Dye, B. A., Wei, L., Thornton-Evans, G. O., & Genco, R. J. (2012). Prevalence of periodontitis in adults in the united states: 2009 and 2010. Journal of Dental Research, 91(10), 914–920. https://doi.org/10.1177/0022034512457373
Parkar, S. M., Shah, K., Darjee, N., & Sharma, A. (2017). Efficacy of ozonated water and chlorhexidine mouth rinse against plaque and gingivitis : A randomized clinical trial, 81–85. https://doi.org/10.4103/2468-6859.204702
Sadatullah, S. (2012). Ozonated water an adjunct to tooth brushing and flossing. Myth or reality?, 1847–1852.
Herring, M. F. S. (2016). Illustrated Anatomy of the Head and Neck 5th Edition.
Life Extension. (2013). Disease Prevention and Treatment.
Mathews, M. J., Mathews, E. H., & Mathews, G. E. (2016). Oral health and coronary heart disease. BMC Oral Health, 16(1), 1–10. https://doi.org/10.1186/s12903-016-0316-7
Mozaffarian, D., Benjamin, E. J., Go, A. S., Arnett, D. K., Blaha, M. J., Cushman, M., … Turner, M. B. (2016). Heart disease and stroke statistics-2016 update a report from the American Heart Association. Circulation (Vol. 133). https://doi.org/10.1161/CIR.0000000000000350
Nogales, C. G., Ferrari, P. H., Kantorovich, E. O., & Lage-Marques, J. (2008). Ozone therapy in medicine and dentistry. Journal of Contemporary Dental Practice, 9(4), 1–9.
Grossman, S. C. (2013). Porth’s Pathophysiology: Concepts of Altered Health States.
Huth, K. C., Quirling, M., Lenzke, S., Paschos, E., Kamereck, K., Brand, K., … Ilie, N. (2011). Effectiveness of ozone against periodontal pathogenic microorganisms. European Journal of Oral Sciences, 119(3), 204–210. https://doi.org/10.1111/j.1600-0722.2011.00825.x
Gupta, G., & Mansi, B. (2012). Ozone therapy in periodontics. Journal of Medicine and Life, 5(1), 59–67. Retrieved from http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3307081&tool=pmcentrez&rendertype=abstract
Seidler, V., Linetskiy, I., Hubálková, H., Stanková, H., Smucler, R., & Mazánek, J. (2008). Ozone and its usage in general medicine and dentistry. A review article. Prague Medical Report, 109(1), 5–13.
Bocci, V. V. (1999). Biological and clinical effects of ozone. Has ozone therapy a future in medicine? British Journal of Biomedical Science, 56(4), 270–279. Retrieved from http://mosao2.org/Article – Bocchi
Deborah Freudenmann has a Bachelor of Health Sciences in Naturopathy and is a co-author and teacher of the Functional Medicine Health Coaching program. She has previously completed a Cert. IV in Food Coaching, Diploma in Holistic Massage Therapy and a Diploma in Anatomy and Physiology. Deborah continues to research, write and educate. With a passion for education Deborah has found her interest discovering and assimilating the newest research and finding ways to apply this research. In doing so Deborah continues to investigate and educate people on understanding, finding and resolving the underlying causation of chronic diseases.
(Taken from https://www.trulyheal.com/can-your-bleeding-gums-lead-to-heart-disease/)